Endometrial Microbiome Test
Endometrial Microbiome Test
Our partner Varinos is the first company in the world to commercialize an Endometrial Microbiome test
The endometrial microbiome test examines the existence of Lactobacillus spp in the endometrium or vagina. There have been report s correlating the existence of Lactobacillus spp in the uterus with pregnancy outcomes.
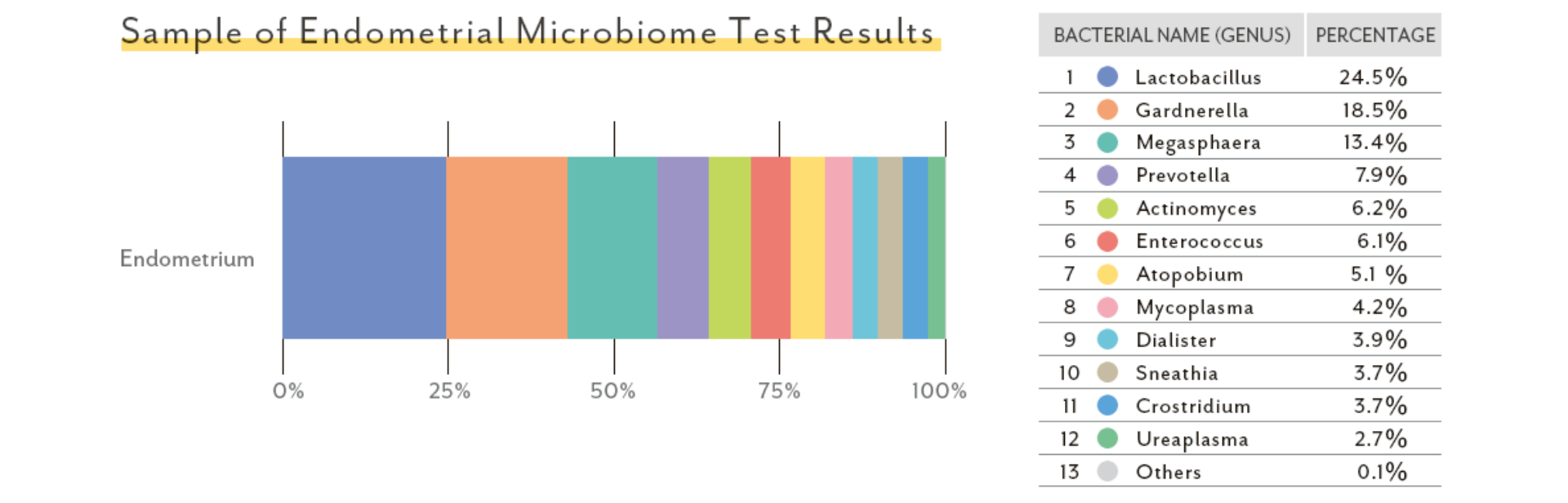
The percentage contributions of other bacterial species are also provided including pathogenic bacterial species. Results are presented in an easy interpret report for assessment of the microbiome makeup of the sample.
Please note that this is not a diagnostic test.
Features
Product Name: Endometrial Microbiome Test
NGS: MiSeq from Illumina
Sample: Fluid
Sample Condition: Room Temperature
No Call Rate:1.5%
Targeted Bacteria: All bacteria (Comprehensive)
Targeted Patients: IVF, RIF, CV, IUI, Pregnant Women
TAT: 4 weeks
Location of Lab: Japan
Components
We will send a test kit containing a pipette and a sample collection tube together with a return envelope.
Storage and Stability
When the sample is collected in the provided sample tube, it will be stable for at least four weeks in room temperature.
Precautions and warnings
The procedure must be performed by a trained clinician.
General recommendations
This test is suitable for:
- Patients with few blastocyst
- IVF RIF (repeated implantation failures)
- RPL (repeated pregnancy loss)
Documents
References
Summary of Publications
The publications indicate the level of Lactobacillus abundance is associated with pregnancy rate.
| No. | Title | Summary | Source |
| 1 | Lactobacillus Dominance in the Endometrium Increases the Success Rate of AIH | Pregnant group exhibited Lactobacillus composition of 90.2% while non pregnant group 70.7% for AIH patients. | Nabeta et al. Journal of Fertilization and Implantation (Tokyo) 38 (1): 76-81, 2021 |
| 2 | Evidence that the microbiota has an effect on implantation
success or failure |
Existence of non-Lactobacillus spp. is correlated with
negative impacts on reproductive function. |
I. Moreno et al, AJOG (2016) |
|
3 |
Analysis of endometrial microbiota by 16S ribosomal RNA gene sequencing among infertile patients: a single-center pilot study | Group with 90%> of Lactobacillus showed 70.7% of pregnancy rate vs group with 90%< of the spp. 33.3%. | K. Kyono et al., Reproductive Health and Biology (2018) |
|
4 |
Endometrial and Vaginal Microbiome Influence ART Outcomes |
The balance between Lactobacillus and pathological bacterial abundance in the endometrial and vaginal microbiomes is associated with pregnancy from ART | M. Miyagi, JBRA Assisted
Reproduction, 2022 |
|
5 |
Analysis of endometrial microbiota by 16S ribosomal RNA gene sequencing among infertile patients: a single-center pilot study | Healthy volunteers presented 99.50% Lactobacillus
composition while 63.90% for IVF patients. |
K. Kyono et al., Reproductive Health and Biology (2018) |
|
6 |
Endometrial microbiota composition is associated with reproductive outcome in infertile patients |
Prospective study to investigate endometrial samples in a cohort of 342 patients indicates endometrial microbiota is a useful biomarker to predict reproductive outcomes. | Moreno et al. Microbiome
(2022) 10:1 |
|
7 |
The influence of vaginal microbiota on frozen blastocyst implantation after transfer: a prospective study through next- generation 16S rRNA sequencing | Vaginal Lactobacillus dominant group with 90%+ shows 73.3% of pregnancy rate while 30% with below 90% of Lactobacillus. | H. Asakura et al. ESHRE 36th Annual Meeting (2021) |
|
8 |
Impact of Lactobacillus in the uterine microbiota on in vitro fertilization outcomes | The implantation rate was significantly lower for those in whom L. iners predominated compared with the others | D. Kadogami, Journal of Reproductive Immunology Volume 160, December 2023 |
|
9 |
Vaginal Microbiota associated with Preterm Delivery | Increased positivity of Ureaplasma species in vaginal microbiota was a risk factor for preterm delivery among women with potential premature labor. | Yutoku Shi, Journal of Infection and Chemotherapy Volume 26, Issue 11, November 2020,
Pages 1134-1138 |
|
10 |
Uterine endometrium microbiota and pregnancy outcome in women with recurrent pregnancy loss |
Increases in Ureaplasma species in uterine endometrial microbiota of women with Recurrent Pregnancy Loss were risks of miscarriage with normal chromosome karyotype and preterm delivery in subsequent pregnancies. |
Yutoku Shi, Journal of Reproductive Immunology Volume 152, Aug. 2022 |
FAQ
Frequently asked questions – Endometrial Microbiome Test (EMT)
What is Endometrial Microbiome?
The endometrial microbiome is a community of microorganisms, primarily bacteria, that reside within the uterus. Similar to the vaginal microbiome, Lactobacillus species typically dominate the endometrial microbiome. Lactobacillus produces lactic acid, creating an acidic environment that inhibits the growth of pathogenic bacteria. This acidic environment helps to maintain a healthy balance of microorganisms within the uterus. Dysbiosis, or an imbalance of the endometrial microbiome, can lead to increased maternal immune activation, making it more difficult to suppress immune responses against the developing embryo and potentially compromising pregnancy outcomes.
Who should test for EMT?
Women experiencing recurrent pregnancy loss, implantation failure, unexplained infertility, or those undergoing assisted reproductive technologies (ART) may benefit from an EMT. Additionally, women with a history of chronic endometritis could consider testing to assess the health of their endometrial microbiome.
Given that the microbial environment significantly influences the implantation process, EMT testing can also be beneficial for women undergoing intrauterine insemination (IUI) to potentially increase success rates.
Why is it better to take the test from the endometrium (endometrial luminal fluid) instead of the vagina?
Recent studies have shown that vaginal and endometrial microbiomes share many similarities, but approximately 20% of patients exhibit distinct bacterial profiles. Sampling directly from the endometrial cavity provides a more accurate representation of the microbial community within the uterus. This specificity is crucial for making appropriate treatment choices.
How can a contamination from the vaginal microbiome be avoided?
To minimize vaginal contamination during endometrial sampling, healthcare providers typically use specialized pipettes designed to collect fluid directly from the endometrial cavity.
Before collection, the vagina and cervical canal should be washed with sterile cotton balls and dried.
There is a possibility of bacteria adhering to the surface of the collection pipette from the cervix. When transferring the sample into the collection tube using the pipette, ensure that the pipette’s surface does not come into contact with the tube, allowing only the collected specimen to be transferred.
Why is an EMT test needed? Can we not, treat directly with antibiotics and Lactobacillus instead without testing?
Antibiotics and probiotics are commonly used to treat endometrial imbalances.
The EMT can identify the specific microorganisms present and their relative abundance and, depending on the test results, suggest examples of appropriate treatment options in combination with antibiotics and supplements.
It goes without saying that it is nonsense to administer antibiotics when the microbiota is normal, and even in dysbiosis it is important to select and treat with the correct antibiotic depending on the species of bacteria detected.
In addition, the indiscriminate use of antibiotics without testing can upset the delicate balance of the microbiome and lead to antibiotic resistance. Additionally, many cases do not improve with treatments based on supplements alone.
Selecting the appropriate antimicrobials according to test results and combining the treatment strategy with supplements is critical in terms of improving implantation rates.
Why is the Varinos test method preferable compared to others?
The Varinos test method offers several advantages over traditional methods, making it a preferred choice for microbial analysis. Here are the key reasons:
- High Sensitivity
- Lower Detection Limit: Varinos tests exhibit exceptionally high sensitivity, meaning they can detect even minute quantities of bacteria that may go undetected by other methods. This increased sensitivity is crucial for identifying low-abundance microorganisms that could be significant in various biological processes.
- Species-Level Identification
- Beyond Genus: Unlike traditional 16S rRNA sequencing, which primarily identifies bacteria at the genus level, Varinos technology allows for species-level identification. This granular level of detail provides more accurate and informative insights into microbial communities.
- Comprehensive and Cost-Effective: Varinos’ proprietary technology enables comprehensive species-level identification at a lower cost compared to other methods, making it a more accessible and cost-effective option for researchers and clinicians.
- Validated by Extensive Research
- Peer-Reviewed Publications: The effectiveness and reliability of the Varinos test method have been extensively validated through numerous peer-reviewed publications. This body of research provides strong evidence supporting the accuracy and precision of the technology.